

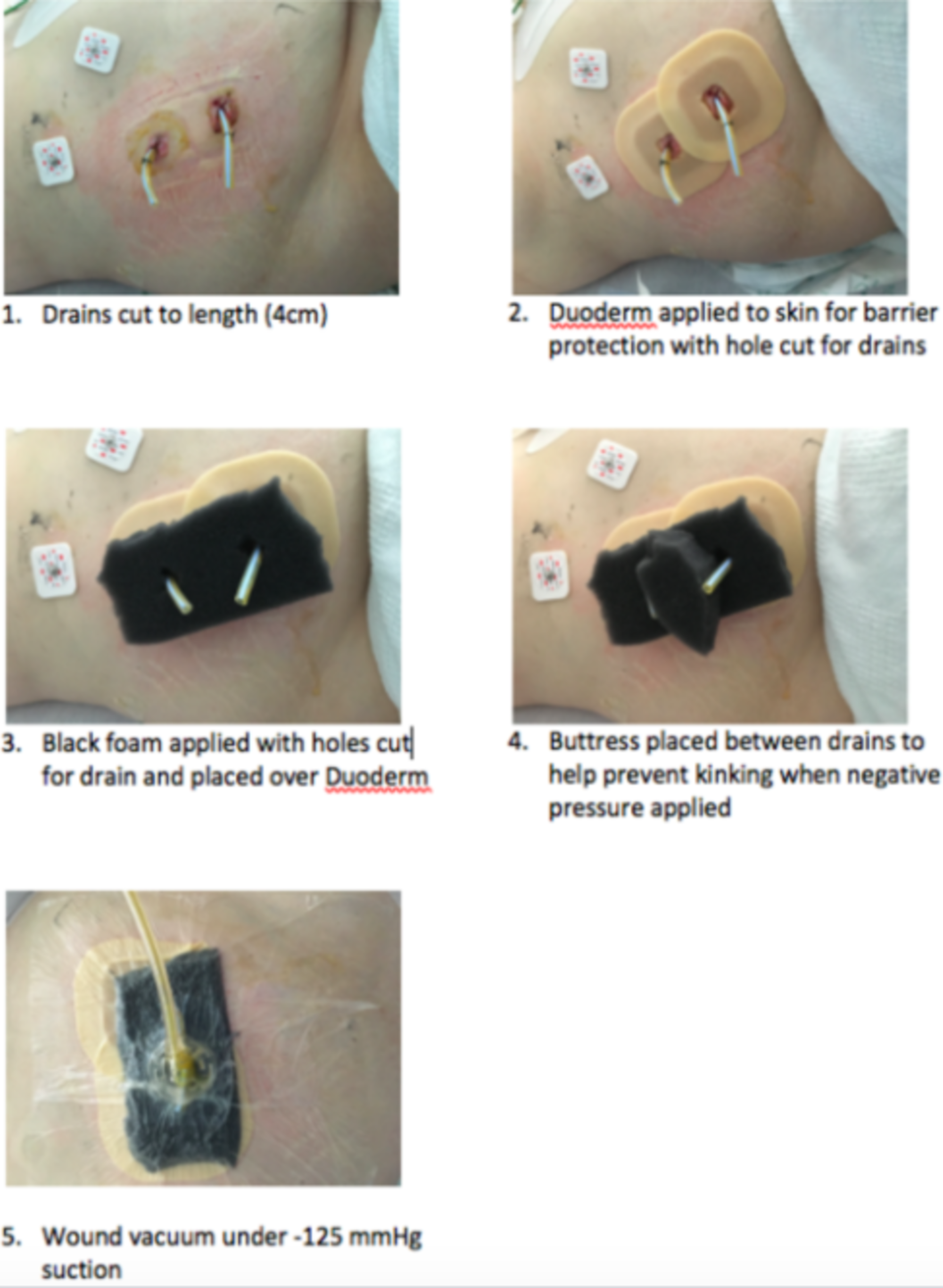
The purpose of this comprehensive review was to give a detailed analysis of the use of NPWT in head and neck cancer patients, as well as to analyze the impact of previous irradiation and other risk factors on patients’ wound healing. Delayed wound healing has its own share of financial burden- and treatment-related delays that significantly impact clinical outcomes. Poor functional status, malnutrition, previously irradiated tissue, and poor oral hygiene contribute to compromised wound healing that requires additional support for wound management. The majority of head and neck cancer patients present at an advanced stage, thus requiring major ablative surgeries and the reconstruction of large defects. This may be attributed to the complexity of anatomical subsites of the head, the neck, and (subsequently) the difficulty of properly adjusting a NPWT dressing. Though NPWT has been used in the management of donor site morbidity in head and neck reconstruction, limited data on its use in head and neck sites have been published. This results in increased tissue perfusion and promotes the formation of a well-granulating wound bed. Adjustable negative pressure applied via an adhesive film over a foam padding promotes wound healing by removing wound exudate and decreasing interstitial edema and bacterial load at the wound site. Negative pressure wound therapy (NPWT) has remained an integral part of wound management for general, orthopedic, and plastic surgeons for more than half a decade. Previous irradiation and DM have detrimental effects on wound healing after NPWT. (4) Conclusion: NPWT treats complex wounds in head and neck cancer patients and should represent a significant armamentarium in head and neck cancers.

Previous irradiation ( p = 0.01 OR = 4.07) and diabetes mellitus (DM) ( p = 0.001 OR = 5.62) were found to be significantly associated with delayed wound healing after NPWT. The median negative pressure recorded was 125 mm of Hg, with a median dressing change time of three days. The overall wound healing response rate was 87.5%.
The neck was found to be the most common site of involvement (47.3%). The most common etiologies requiring NPWT were defects post tumor resection and flap reconstruction and oro/pharyngo-cutaneous fistulas. (3) Results: 15 studies fulfilled the inclusion criteria. (2) Material and Methods: We conducted a comprehensive search in PubMed, Medline, Embase, Web of Science, and Cochrane Library databases for relevant literature. The purpose of this study was to provide an evidence-based review of NPWT in head and neck cancer patients, as well as the impact of previous irradiation and other risk factors on wound healing. (1) Background: Negative pressure wound therapy (NPWT) has been effectively used for wound management in comparison to traditional dressings.


 0 kommentar(er)
0 kommentar(er)
